IBS vs. IBD: Understanding the Differences and How to Manage Them
If you’ve ever struggled with digestive issues, you may have come across the terms IBS (Irritable Bowel Syndrome) and IBD (Inflammatory Bowel Disease). While these two conditions share some similar symptoms, they are fundamentally different in causes, severity, and long-term health implications.
The confusion between IBS vs. IBD is common, and understandably so since both can lead to abdominal discomfort, irregular bowel movements, and a significant impact on daily life. However, IBS is a functional disorder that affects how the gut works, while IBD is an inflammatory disease that causes lasting damage to the digestive tract.
Understanding the differences between IBS vs. IBD is essential for proper diagnosis, management, and treatment. In this article, we’ll break down the key distinctions, symptoms, causes, and treatment options to help you navigate these conditions with confidence.
What is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder, meaning it affects the way the gut functions rather than causing structural damage or inflammation. Unlike conditions such as Inflammatory Bowel Disease (IBD), IBS does not cause visible damage to the intestines but can still lead to significant discomfort and digestive disturbances.
If you want a deeper dive into IBS, including its symptoms, triggers, and management strategies, check out my previous blog about IBS.
Common Symptoms of IBS
IBS presents differently from person to person, but the most common symptoms include:
Abdominal pain or cramping (often relieved after a bowel movement).
Bloating and excessive gas.
Changes in bowel habits, including diarrhea (IBS-D), constipation (IBS-C), or alternating between both (IBS-M).
Mucus in stool (without blood).
These symptoms tend to fluctuate, often triggered by food, stress, or hormonal changes.
Possible Causes of IBS
The exact cause of IBS is not fully understood, but several factors may contribute to its development, including:
Gut-brain axis dysfunction – The communication between the brain and gut may be disrupted, leading to changes in gut motility and sensitivity.
Stress and mental health conditions – Anxiety, depression, and stress can exacerbate IBS symptoms.
Food intolerances – Certain foods, such as dairy, gluten, high-FODMAP foods, and artificial sweeteners, may trigger symptoms.
Gut microbiome imbalances – An imbalance in the gut bacteria (dysbiosis) may play a role in IBS development.
Diagnosing IBS: The Rome IV Criteria
Since IBS doesn’t cause structural damage, there is no single test to diagnose it. Instead, doctors rely on the Rome IV criteria, which include:
Recurrent abdominal pain for at least one day per week in the last three months, associated with:
Changes in stool frequency
Changes in stool form (diarrhea, constipation, or both)
Relief or worsening of symptoms after a bowel movement
Doctors may also conduct additional testing—such as stool samples, blood tests, and colonoscopies—to rule out other conditions like IBD or celiac disease.
IBS Does Not Cause Inflammation or Structural Damage
One of the key differences between IBS vs. IBD is that IBS does not cause inflammation, ulcers, or long-term damage to the digestive tract. While symptoms can be uncomfortable and impact quality of life, IBS is considered a chronic but manageable condition.
What is Inflammatory Bowel Disease (IBD)?
Inflammatory Bowel Disease (IBD) is a chronic autoimmune condition that causes inflammation and damage to the digestive tract. Unlike IBS, which affects gut function, IBD results in visible inflammation, ulcers, and structural changes in the intestines. Because of its chronic and progressive nature, IBD requires long-term management and, in some cases, medical interventions such as immunosuppressants or surgery.
Types of IBD: Crohn’s Disease vs. Ulcerative Colitis
There are two main types of IBD:
Can affect any part of the digestive tract, from the mouth to the anus.
Inflammation occurs in multiple layers of the intestinal walls.
Symptoms may include patchy areas of inflammation, leading to complications like strictures (narrowing of the intestines) or fistulas (abnormal connections between tissues).
Affects only the colon (large intestine) and rectum.
Inflammation is continuous and limited to the inner lining of the colon.
Symptoms are typically more consistent and may involve frequent, urgent bowel movements.
Common Symptoms of IBD
The symptoms of IBD vary depending on whether a person has Crohn’s disease or ulcerative colitis, but they often include:
Persistent diarrhea (often severe and chronic).
Blood in the stool (due to inflammation and ulcers in the digestive tract).
Abdominal cramping and stomach pain.
Unintended weight loss and poor nutrient absorption.
Fatigue and low energy levels, often due to inflammation and anemia.
What Causes IBD?
The exact cause of IBD remains unknown, but research suggests that it may develop due to a combination of genetic, immune, and environmental factors:
Overactive immune system – The body’s immune system mistakenly attacks the digestive tract, leading to chronic inflammation.
Genetics – A family history of IBD increases the risk of developing the condition.
Environmental triggers – Diet, stress, infections, and gut microbiome imbalances may contribute to disease flare-ups.
How is IBD Diagnosed?
Because IBD causes physical damage and inflammation in the intestines, doctors use a combination of tests to confirm a diagnosis:
Colonoscopy and endoscopy – To examine the digestive tract for ulcers, inflammation, and damage.
Imaging tests (CT or MRI scans) – To detect inflammation or strictures in the intestines.
Blood tests – To check for markers of inflammation and anemia.
Stool tests – To rule out infections or determine levels of inflammatory markers (such as calprotectin).
Unlike IBS, which affects gut function without causing damage, IBD is an inflammatory condition that can lead to long-term complications if not properly managed. Early diagnosis and treatment are essential to prevent disease progression and improve quality of life.
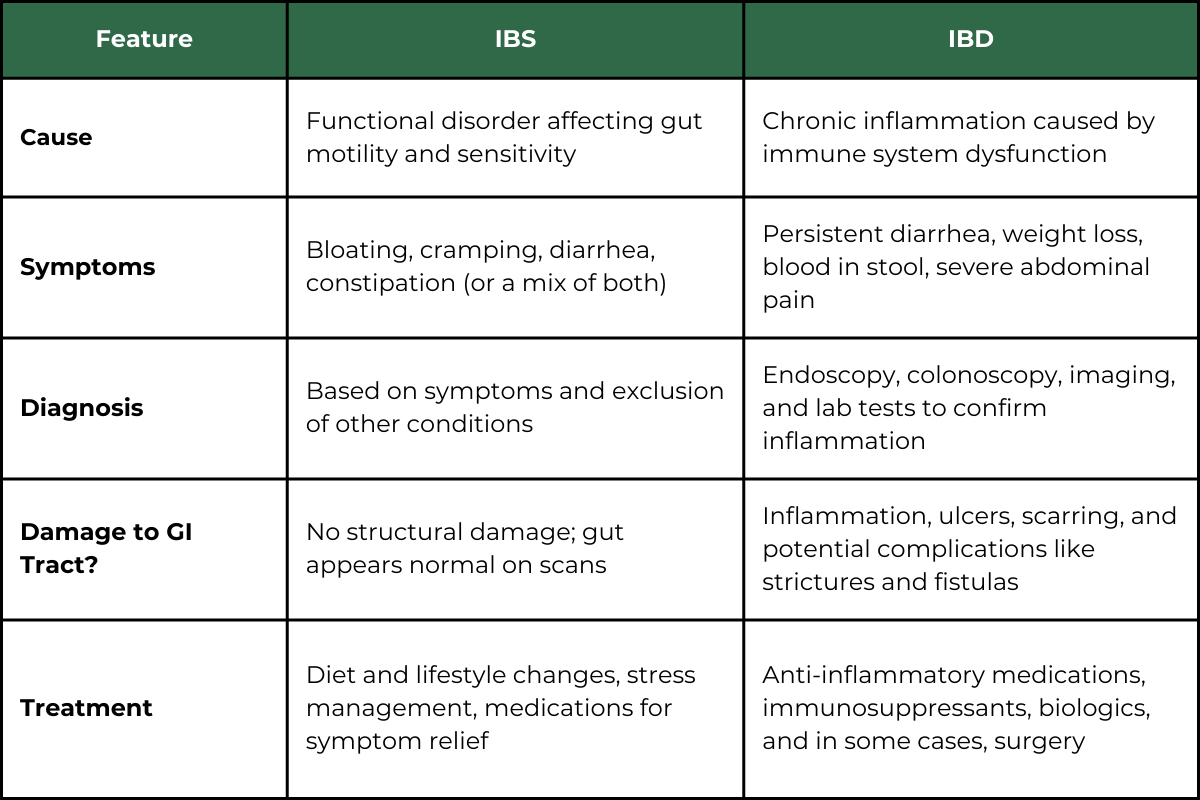
IBS vs. IBD: Key Differences
Although IBS and IBD both affect the digestive system and share some overlapping symptoms, they are fundamentally different conditions with distinct causes, diagnoses, and treatment approaches.
The table below provides a side-by-side comparison of IBS vs. IBD:
Why These Differences Matter for Treatment
Understanding the distinction between IBS vs. IBD is critical because the approach to managing each condition is vastly different:
IBS is treated by managing symptoms through diet, stress reduction, probiotics, and medications that regulate gut motility (e.g., antispasmodics or laxatives). Since IBS doesn’t cause inflammation, anti-inflammatory drugs are not typically needed.
IBD requires medical intervention to reduce inflammation and prevent complications. Treatment often includes immune-modulating medications, corticosteroids, and biologics, with surgery sometimes necessary for severe cases.
A Misdiagnosis Can Lead to the Wrong Treatment Plan
Many people with persistent digestive symptoms may assume they have IBS when they could actually have IBD. If symptoms include blood in the stool, unintentional weight loss, or severe fatigue, it’s important to see a doctor to rule out IBD or other serious conditions.
By recognizing the differences between IBS and IBD, individuals can take the right steps toward effective management and long-term gut health.
How are IBS and IBD Treated?
Since IBD and IBS have different causes, their treatment strategies are also distinct. IBS treatment focuses on managing symptoms and improving gut function, while IBD treatment aims to control inflammation and prevent complications.
IBS Treatment Options
IBS is managed through lifestyle changes, dietary modifications, and symptom-relief medications, as there is no structural damage to heal.
Dietary Changes
Low FODMAP diet – Reducing fermentable short-chain carbohydrates that can trigger bloating and digestive discomfort. Many people find success with a Low FODMAP Mediterranean Diet, which combines gut-friendly foods with the health benefits of the Mediterranean diet. If you’d like to explore this approach, check out my previous blog: Low FODMAP Mediterranean Diet: A Guide for IBS Sufferers. Need help getting started with the Low FODMAP Diet? Download my Free Low FODMAP Guide here.
Fiber modifications – Soluble fiber (e.g., psyllium) can help with constipation-predominant IBS, while insoluble fiber may worsen symptoms in some cases.
Stress Management
Mindfulness, meditation, and deep breathing can help reduce stress-related flare-ups.
Gut-directed hypnotherapy has shown promise in improving symptoms by addressing the gut-brain connection.
Probiotics and Gut Microbiome Support
Certain probiotic strains (such as Bifidobacterium and Lactobacillus) may help regulate gut bacteria and reduce bloating.
Medications for Symptom Relief
Antispasmodics (e.g., peppermint oil, dicyclomine) help with cramping.
Laxatives or stool softeners for constipation-predominant IBS (IBS-C).
Anti-diarrheal medications (e.g., loperamide) for diarrhea-predominant IBS (IBS-D).
Since IBS is highly individualized, treatment is often trial and error, focusing on lifestyle adjustments and symptom management rather than medical intervention. If you’re looking for practical ways to manage IBS on a daily basis, check out my blog: Living with IBS: 7 Practical Tips for Managing IBS Symptoms Daily.
IBD Treatment Options
Unlike IBS, IBD requires medical treatment to control inflammation and prevent complications like intestinal strictures or fistulas.
Medications
Anti-inflammatories – 5-ASA drugs (e.g., mesalamine) help reduce inflammation in the gut lining.
Corticosteroids – Used for short-term relief during flare-ups but not for long-term management due to side effects.
Immunosuppressants – Help regulate the immune system’s response to prevent excessive inflammation.
Biologics – Target specific inflammatory pathways and are often used when other treatments fail.
Nutritional Support and Anti-Inflammatory Diets
Certain diets (e.g., Mediterranean, Specific Carbohydrate Diet, anti-inflammatory diets) may help reduce symptoms and promote gut healing.
Nutritional supplementation (such as iron, vitamin B12, and vitamin D) may be needed for those with malabsorption.
Lifestyle Modifications
Regular movement, stress reduction, and adequate sleep can help manage symptoms and improve quality of life.
Surgery (in Severe Cases)
In ulcerative colitis, a colectomy (removal of part or all of the colon) may be necessary for severe cases.
In Crohn’s disease, bowel resection surgery may be needed to remove damaged sections of the intestines.
While IBD and IBS both affect the digestive system, their treatments are vastly different. IBS is managed through diet, stress management, and symptom relief, while IBD requires medical intervention to control inflammation and prevent complications.
When to See a Doctor
If you’re experiencing digestive discomfort, you might be wondering whether it’s IBS or something more serious like IBD. While IBS symptoms can be disruptive, they don’t cause permanent damage. IBD, on the other hand, involves chronic inflammation that can lead to serious complications if left untreated.
Warning Signs that Require Medical Attention
If you experience any of the following symptoms, it’s important to see a doctor as soon as possible:
Blood in your stool or rectal bleeding – This can indicate inflammation, ulcers, or bleeding in the digestive tract, which is not typical of IBS. If you notice bright red blood (which may suggest rectal bleeding) or dark, tarry stools (which may indicate bleeding higher up in the digestive tract), consult a doctor immediately.
Unexplained weight loss – Significant weight loss without changes in diet or exercise may suggest malabsorption, a common issue in IBD.
Chronic abdominal pain – While IBS can cause discomfort, intense, unrelenting pain may signal something more serious.
Chronic diarrhea (lasting more than a few weeks) – If you experience frequent, watery stools, especially with blood or mucus, it could be a sign of IBD.
Fatigue and anemia – If you feel constantly exhausted, lightheaded, or notice paleness in your skin, it could be due to chronic inflammation and nutrient deficiencies.
Fever or night sweats – These symptoms are not typical of IBS and could indicate an inflammatory condition like IBD.
The Importance of an Accurate Diagnosis
Since IBS and IBD share some overlapping symptoms, self-diagnosing can lead to mismanagement and ineffective treatment. IBS can often be managed with diet and lifestyle changes, while IBD requires medical intervention to prevent complications.
A healthcare provider can perform tests such as blood work, stool analysis, imaging, or a colonoscopy to determine whether your symptoms are due to IBS, IBD, or another digestive condition like celiac disease.
If you’re struggling with ongoing digestive issues, don’t ignore them—seeking medical advice can help you get the right diagnosis and an effective treatment plan.
Final Thoughts: Understanding IBS vs. IBD for Better Gut Health
While IBS and IBD share some symptoms, they are fundamentally different conditions that require distinct approaches to management and treatment. IBS is a functional disorder that affects how the gut works but doesn’t cause inflammation or lasting damage. IBD, on the other hand, is a chronic autoimmune condition that leads to inflammation, ulcers, and potential complications if not properly treated.
Take Control of Your Gut Health
If you’ve been struggling with digestive issues and are unsure whether it’s IBS or IBD, it’s important to get an accurate diagnosis so you can follow the right treatment plan.
👉 Need help managing IBS symptoms? Check out my Free Low FODMAP Guide for simple dietary strategies that can make a big difference!
👉 If your symptoms are persistent or worsening, consult a healthcare professional to determine the best approach for your gut health.